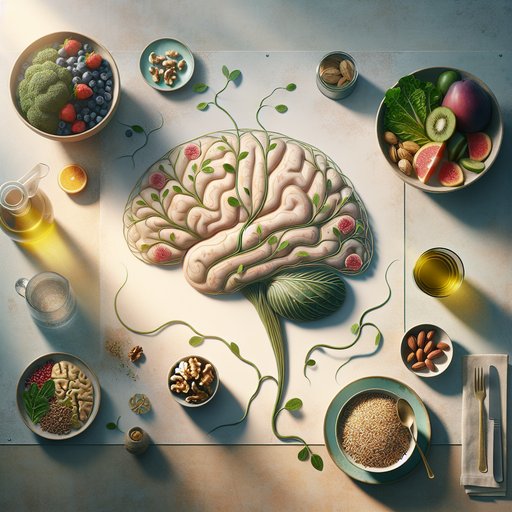
As life expectancy rises, protecting brain function has become a central health goal. Diet is one of the most practical levers we can pull: it shapes vascular health, fuels synapses, and influences inflammation and the microbiome, all of which matter for memory and attention. A growing body of research now moves beyond vague notions of “healthy eating” to examine specific foods and patterns that track with better cognition in older adults. While nutrition is not a treatment for disease, evidence-informed choices—made consistently—can support long-term mental sharpness, complementing sleep, exercise, and social engagement. This article distills the latest findings into actionable strategies you can take to your kitchen and your clinician, helping you build a brain-friendly plate without hype.
We are living longer than any generation before us, but age-related cognitive decline is rising alongside modern challenges like sedentary lifestyles, ultra-processed diets, and metabolic disease. Diet intersects with brain health through multiple pathways: it influences blood flow to the brain, modulates oxidative stress and inflammation, and helps maintain glucose control that stabilizes energy to neurons. Because these mechanisms accumulate over decades, everyday food choices meaningfully shape risk trajectories for later-life memory and executive function. Focusing on specific foods with the strongest evidence provides practical guidance that cuts through conflicting headlines.
Two dietary patterns dominate the research landscape: the Mediterranean-style diet and the MIND diet, which blends Mediterranean principles with brain-focused choices such as leafy greens and berries. Long-term observational studies link higher adherence to both patterns with slower cognitive decline and lower dementia risk. Randomized trials add nuance: sub-studies of a Mediterranean intervention enriched with extra-virgin olive oil or walnuts reported better cognitive performance than a lower-fat control, while a recent MIND-diet trial did not outperform an active comparison over three years, possibly reflecting shared weight loss and lifestyle support in both groups. Together, these data suggest patterns matter, but their benefits likely flow from repeated exposure to specific foods.
That makes the shopping list—not just the label on the diet—critical. Leafy green vegetables are among the most consistently associated foods with slower cognitive aging. In cohort research, older adults who ate a daily serving of spinach, kale, collards, or similar greens experienced substantially slower rates of decline than peers who rarely ate them. Mechanistically, these foods deliver folate and vitamin K, plus carotenoids such as lutein and zeaxanthin—pigments found in brain tissue that may support neuronal efficiency.
Small randomized trials of lutein and zeaxanthin supplementation report modest improvements in aspects of memory and processing speed, reinforcing the plausibility of food-based benefits. A practical move is to make one generous serving of greens a daily habit, sautéed with olive oil to enhance carotenoid absorption. Berries and cocoa are rich in flavanols, a class of polyphenols that appears to support memory through improved blood vessel function and signaling in the hippocampus. Controlled trials with blueberries and mixed berry powders have shown modest gains in verbal memory and executive tasks in older adults over weeks to months.
In 2023, a large randomized study reported that adults with low baseline flavanol intake improved on a hippocampal-dependent memory test after daily flavanol supplementation, while those already consuming adequate amounts saw little change. Translation to the plate favors minimally sweetened options: fresh or frozen berries several times per week and unsweetened cocoa (or high-cocoa, low-sugar dark chocolate) used in yogurt or oatmeal rather than high-sugar desserts. Fatty fish provide long-chain omega-3s, especially DHA, a structural component of neuronal membranes that influences synaptic function. Observational studies repeatedly associate higher fish intake with better cognitive trajectories, and trials of omega-3 supplements show mixed but generally more favorable results in people with low fish consumption or early cognitive concerns.
Beyond direct neural effects, fish-rich meals tend to displace processed meats and refined foods, improving vascular and metabolic profiles that matter for the brain. Aim for one to two servings per week of lower-mercury choices like salmon, sardines, trout, or herring, and consider algal-derived DHA if you avoid fish. Whole-food sources deliver additional nutrients such as selenium, iodine, and vitamin D, though supplementation may be appropriate for documented deficiencies. Metabolic and vascular stability are essential for cognitive aging, and here everyday staples carry weight.
Meals built from whole grains, legumes, vegetables, nuts, and extra-virgin olive oil blunt post-meal glucose spikes and provide fiber that feeds gut microbes, producing short-chain fatty acids with anti-inflammatory effects. Fermented foods such as yogurt, kefir, kimchi, and sauerkraut have been shown in randomized trials to increase microbiome diversity and reduce inflammatory markers; while cognitive outcomes are still under study, this pathway is biologically plausible. Conversely, higher intake of ultra-processed foods has been linked in large cohorts with lower cognitive scores and faster decline, a pattern likely mediated by excess sugar, sodium, additives, and poor nutrient density. Coffee and tea, when consumed in moderation and timed to protect sleep, are associated with lower risk of cognitive decline in observational research, potentially via caffeine’s acute attentional benefits and polyphenols’ vascular effects.
Putting these findings into a weekly routine works best when guided by repetition rather than perfection. Make leafy greens a daily anchor, rotate berries several times per week, and feature a fatty fish meal once or twice weekly alongside beans or whole grains. Cook primarily with extra-virgin olive oil, keep a handful of unsalted nuts as a regular snack, and add fermented foods you enjoy and tolerate. Replace sugary desserts with fruit or unsweetened cocoa preparations, and swap refined starches for intact grains to steady energy.
Frozen produce, canned fish, and prewashed greens are cost- and time-savvy tools that preserve nutrient quality while lowering barriers to consistency. Personalization matters, and small adjustments can make brain-friendly eating sustainable. If you have diabetes, kidney disease, or digestive conditions, work with a registered dietitian or healthcare professional to tailor fiber, potassium, and carbohydrate choices. If you do not eat fish, discuss algal DHA and B12 status; if you are considering supplements like flavanols or carotenoids, remember that most benefits in trials are modest and often smaller than what long-term dietary patterns confer.
Alcohol does not earn a place for brain health, as any potential benefit is outweighed by known risks; prioritizing hydration, sleep-friendly caffeine timing, and minimally processed foods is a safer bet. Diet is powerful, but it is most effective when paired with physical activity, cognitive engagement, and social connection. The evidence will continue to evolve, yet the core direction is consistent: emphasize plants, prioritize polyphenol-rich produce, include marine or algal omega-3s, choose extra-virgin olive oil and nuts for fats, cultivate a healthy microbiome, and minimize ultra-processed foods. These choices support the same systems—vascular, metabolic, and inflammatory—that keep the brain resilient.
Think in meals and months, not hacks and days; the brain rewards steady patterns more than occasional superfoods. For individualized guidance, especially if you manage medical conditions or take medications, consult your healthcare team. With a few strategic staples and an eye on consistency, you can stack the odds in favor of mental clarity across the decades.